ectropion Loss of elasticity or control of the eyelid, usually the lower eyelid, that causes it to sag away from the EYE. Ectropion allows tears to over- flow the lid rather than remaining in the eye. It also fails to protect the eye, and especially the CORNEA, permitting dryness and exposure to environmental particles that create irritation and possibly injury to the cornea and sclera (“white” of the eye). Common causes of ectropion include
• aging
• damage to the nerves that control the eyelids
• CICATRICIAL PEMPHIGOID
Ectropion is a common symptom of BELL’S PALSY, a temporary paralysis of one side of the face that results from INFLAMMATION of the seventh cranial NERVE (facial nerve), and also may accompany neurologic disorders such as PARKINSON’S DISEASE and MULTIPLE SCLEROSIS.
With ectropion the eye feels irritated and scratchy. Tear production becomes excessive as the eye attempts to lubricate and protect itself, and tears typically run over the lip of the lid and onto the cheeks. The doctor can diagnose ectropion based on its appearance. Treatment is typically surgery to tighten the lid structure to permit the lid to stay against the eye. Whether the ectropion recurs depends on the underlying cause. Untreated ectropion may result in extensive dam- age to the surface of the eye and cornea, including INFECTION, that interferes with vision and the health of the eye.
See also AGING, VISION AND EYE CHANGES THAT OCCUR WITH; CONJUNCTIVITIS; CORNEAL INJURY; CRANIAL NERVES; ENTROPION; KERATITIS.
electroretinography A test that measures the electrical activity of the RETINA’s rods and cones in response to light stimulation. The ophthalmologist places anesthetic drops in the EYE to numb it, then attaches an electrode to the surface of the CORNEA. The electrode detects electrical impulses on the retina when the ophthalmologist flashes a beam of light onto the retina, and sends signals to the electroretinograph machine. An electroretinogram is the recording the machine makes of the retina’s responses. Electroretinography helps diagnose dis- orders of the retina such as RETINAL DETACHMENT and RETINITIS PIGMENTOSA.
See also DARK ADAPTATION TEST; RETINOPATHY; SLIT LAMP EXAMINATION.
entropion Deformity of the eyelid in which the lip of the lid, including the eyelashes, curls inward toward the EYE. Scarring that results from CICATRI- CIAL PEMPHIGOID (an AUTOIMMUNE DISORDER in which painful blisters repeatedly form on the insides of the eyelids) or recurrent CONJUNCTIVITIS (INFLAMMA- TION or INFECTION of the inner lining of the eyelids) is a common cause of entropion. Entropion may also develop for unknown reasons (idiopathic). The ophthalmologist can diagnose entropion by its presentation. The irritation of the lid and lashes against the surface of the eye is painful and can cause significant damage to the CORNEA, resulting in VISION IMPAIRMENT and perhaps the need for CORNEAL TRANSPLANTATION. Treatment seeks to relieve the irritation. In mild entropion, lubricating eye drops may be sufficient to protect the eye. Moderate to severe entropion requires surgery to restore the eyelid to its appropriate structure. Once corrected, entropion usually does not recur. See also CORNEAL INJURY; ECTROPION; KERATITIS.
enucleation Surgical removal of a cancerous EYE or a severely diseased or damaged eye. The OPERA- TION, performed under general ANESTHESIA, takes about an hour. After removing the eye, the surgeon places an implant to fill the shape of the socket and provide a means of attaching a PROSTHETIC EYE. A pressure dressing stays in place over the eye orbit for one to two days to minimize swelling and allow the implant to become firmly rooted in the conjunctival tissue. During this time it is common as well as frightening for people to have difficulty opening the other eye, as the eyes are accustomed to functioning together. Once the bandage comes off and the eyelid of the operated eye is free to move, the eyelid for the unoperated eye resumes normal functioning. Complete HEALING takes about six weeks, during which time it is necessary to place anti-inflammatory and antibiotic drops in the operated eye socket to keep swelling and the risk for INFECTION to a minimum.
Though the operation is uncomplicated and the body quickly heals following the surgery, enucleation can be a difficult procedure for people to accommodate emotionally. Even when the eye has been visionless for a long time, the prospect of losing the eye troubles many people. The modern prosthetic eye is typically such a close match for the remaining eye that it is unapparent to other people. Once the operative site heals, the eye orbit (socket) and implant require little care or attention beyond cleaning the external eyelid area for hygienic purposes.
See also ANTIBIOTIC MEDICATIONS; RETINOBLASTOMA; SURGERY BENEFIT AND RISK MANAGEMENT; VISION IMPAIRMENT.
episcleritis INFLAMMATION of the episclera, the membrane that covers the sclera (fibrous outer layer, the “white,” of the EYE). Most episcleritis is idiopathic (occurs for unknown reasons), though the condition sometimes accompanies AUTOIMMUNE DISORDERS such as RHEUMATOID ARTHRITIS and
REITER’S SYNDROME. Episodes are self-limiting though may recur over time, with each episode of inflammation generally lasting 7 to 10 days. Symptoms may include mild irritation and red- ness, and occasionally a nodule (bump) on the surface of the sclera. The doctor can diagnose episcleritis by its appearance. Lubricating eye drops
help relieve the irritation until the inflammation subsides. This is usually the only treatment necessary. Some studies suggest a correlation between episcleritis and hormonal shifts such as occur with the MENSTRUAL CYCLE or MENOPAUSE. Episcleritis is three times more common in women than men. Episcleritis does not affect vision or result in any long-term effects on the health of the eye.
See also CONJUNCTIVITIS; KERATITIS; SCLERITIS.
exophthalmos Bulging outward of the EYE, sometimes called poptosis. Most exophthalmos results from Graves’s disease and is a classic symptom of this form of HYPERTHYROIDISM. Thyroid- related exophthalmos results from swelling of the tissues around the eye and within the orbit that develops in reaction to the high levels of thyroid HORMONE present in the circulation. Other causes of exophthalmos include ORBITAL CELLULITIS, the autoimmune disorder Wegener’s granulomatosis, and FRACTURE of the facial or orbital bones that push the eye out of place. Less common causes of exophthalmos include tumors of the eye, OPTIC NERVE, or BRAIN that protrude into the orbital socket and ANEURYSM (ballooning of the arterial wall) of the internal carotid ARTERY, a branch of which runs behind the eye. Exophthalmos can affect one eye (unilateral) or both eyes (bilateral), and when bilateral can affect one eye more prominently than the other.
Exophthalmos can cause significant and permanent vision impairment, and requires prompt treatment.
The diagnostic path begins with an OPHTHALMO- LOGIC EXAMINATION and blood tests to assess thyroid function. When Graves’s disease or hyperthyroidism is the cause, treatment to restore appropriate levels of thyroid hormones often though not always returns the eye to its normal position. Persistent exophthalmos may prevent the eyelids from closing over the eye, exposing the CORNEA to excessive dryness and potential trauma. Untreated exophthalmos results in VISION IMPAIRMENT that can progress to blindness.
See also AUTOIMMUNE DISORDERS; GRAVES’S OPH- THALMOPATHY.
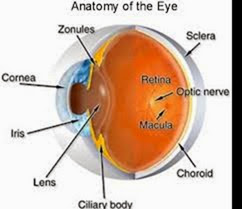
eye The organ of vision. The paired eyes work in coordination to present NERVE impulses the BRAIN interprets as dimensional (stereovisual) images. The function of sight requires close integration among the structures of the eye, the neurologic sys- tem, and the muscular system. Each eye is a fluid-detect color (cones) and brightness (rods). These cells convert the light to nerve impulses that con- verge at the back of the retina at the optic disk, their portal to the optic nerve. The optic nerve conveys the signals to the brain, which interprets them as images.
filled, elongated globe of fibrous tissue, about 1⁄4 inch from front to back and 1 inch from top to bot- tom and side to side, contained within the protective cavity of the orbital socket in the skull. The OPTIC NERVE, the second cranial nerve, provides a direct pathway from the back of the eye to the brain. Six muscles move each eye up and down, from side to side, and in rotation. These muscles direct the eye toward objects within the VISUAL FIELD and hold the eyes steady.
The process of vision begins when lightwaves enter the eye through the CORNEA, a transparent portion of the eye’s tough outer layer, the sclera. The cornea’s convex front surface initially refracts the lightwaves for preliminary focusing. The cornea is soft and flexible but fixed; it does not adjust or move. The LENS, a transparent and flexible convex disk behind the cornea, further refracts the lightwaves. Tiny muscles at the edge of the lens, the ciliary muscles, cause the lens to thicken or flatten to adjust the degree of refraction for optimal focus. The resulting light pattern strikes the RETINA, activating the specialized cells that
detect color (cones) and brightness (rods). These cells convert the light to nerve impulses that converge at the back of the retina at the optic disk, their portal to the optic nerve. The optic nerve conveys the signals to the brain, which interprets them as images.
For further discussion of the eye within the context of ophthalmologic structure and function please see the overview section “The Eyes.” See also AGING, VISION AND EYE CHANGES THAT OCCUR WITH; CRANIAL NERVES.
eye pain
Sensations discomfort involving the EYE and its supporting structures. Eye PAIN may vary
from scratchy irritation to intense and debilitating pain. Much eye pain in the form of burning and itching arises from minor and treatable causes that affect the structures around the eye rather than the eye itself. Eye pain that is throbbing, stabbing, deep, or accompanies visual disturbances may suggest conditions such as GLAUCOMA.
Eye pain that is sudden and severe, accompanies partial or complete loss of vision, prevents movement of the eye, or follows TRAUMA TO THE EYE or face requires emergency medical attention. When there is the possibility of penetrating eye injury, loosely patch both eyes to minimize movement.
The diagnostic path begins with careful examination of both eyes, which may include OPHTHAL- MOSCOPY, FLUORESCEIN STAINING when the doctor suspects CORNEAL INJURY, TONOMETRY to measure the pressure inside the eye, and SLIT LAMP EXAMINATION for further assessment of the RETINA and other structures of the inner eye. The doctor may place an anesthetic medication (numbing eye drops) in the eye to determine whether the pain is coming from the surface of the eye, in which case the pain will go away, or from within the eye, in which case the pain will persist. Often the doctor will also conduct basic tests of VISUAL ACUITY such as a SNELLEN CHART reading.
People who wear contact lenses should remove them at the first sign of discomfort. Treatment for eye pain targets the underlying cause. Most minor causes resolve without complications or permanent VISION IMPAIRMENT. Causes such as severe corneal injury (BURNS, lacerations), glaucoma, and ORBITAL CELLULITIS seriously threaten vision and can result in permanent and complete vision loss without urgent and appropriate treatment.
See also RETINAL DETACHMENT.
eye strain The sensation of tiredness and irritation of the eyes, often accompanying long periods of time involved in performing the same task such as reading, computer work, watching television, playing video games, and assembly work. EYE strain generally results from overuse of the muscles that move the eyes. The overuse tires the muscles, which become less responsive to the focusing needs of the eyes. The difficulty generates temporary vision disturbances such as blurring, and may also cause muscle tension headaches. Insufficient blinking, which causes the eyes to become dry and irritated, often accompanies the overuse.
These measures can help relieve eye strain:
• Blink frequently.
• Use artificial tears to improve the moisture con- tent of the eyes.
• Make sure lighting is of the appropriate intensity and placement.
• Reduce glare and reflection.
• Look away from close tasks every 10 to 15 minutes to focus on objects in the distance.
• Wear reading glasses or CORRECTIVE LENSES to accommodate PRESBYOPIA.
• Wear eye protection when in environments that are dusty or windy, and when in the sun.
Contrary to popular belief, eye strain (such as reading in dim light) does not cause permanent VISION IMPAIRMENT. However, eye strain may result from undetected vision impairment, such as ASTIG- MATISM and HYPEROPIA, that affect the eye’s ability to focus on near objects. An ophthalmologist or optometrist should evaluate eye strain that persists despite efforts to improve the visual environment.
See also ERGONOMICS; HEADACHE; MUSCLE; OCCUPA- TIONAL HEALTH AND SAFETY; VISION HEALTH.