ocular herpes simplex An INFECTION of the eyes with HERPES SIMPLEX VIRUS 1 (HSV-1), which causes cold sores, or herpes simplex virus 2 (HSV-2), which causes GENITAL HERPES. The virus spreads to the eye to cause the initial infection via contamination from contact with an existing herpes sore elsewhere on the body. Ocular herpes simplex features similar eruptions of sores on the surface of the EYE and inside the eyelids. The sores are very painful and can cause permanent scarring of the CORNEA.
About half of people who have one outbreak of ocular herpes simplex will experience a second; about 20 percent have persistently recurring infections, ranking ocular herpes simplex as the leading infectious cause of corneal destruction. A serious complication of ocular herpes simplex is stromal KERATITIS, in which the IMMUNE SYSTEM begins to attack the stromal cells that make up the cornea. This leads to scarring deep within the cornea, resulting in distortions of vision and diminished VISUAL ACUITY.
The sores of ocular herpes simplex are characteristic of the infection. The antiviral medication acyclovir may reduce the severity of outbreaks of the infection when taken at the first sign of symptoms. Some studies show that taking acyclovir for 12 months significantly reduces recurrent ocular herpes simplex. However, there is no cure for herpes infection. Damage that occurs as a consequence of infection is permanent. Infection- control methods, such as frequent HAND WASHING and keeping the fingers away from the eyes, can help prevent initial infection.
See also ANTIVIRAL MEDICATIONS; AUTOIMMUNE DIS- ORDERS; COLD SORE; CORNEAL INJURY; CORNEAL TRANS– PLANTATION.
ocular herpes zoster INFECTION of the eyes with the varicella zoster VIRUS, a member of the HERPES SIMPLEX family of viruses that causes CHICKENPOX and shingles. After the infectious stage of chicken- pox subsides, the virus submerges itself in NERVE roots. It may reemerge years to decades later, erupting in a rash of painful blisters along a nerve tract that hosts the virus. Ocular herpes zoster occurs when an outbreak that affects the face, usually along the tract of the trigeminal nerve, spreads to the EYE. Usually the outbreak affects only the eye on the same side of the face as the shingles eruption, though sometimes the shingles eruption affects both sides of the face. When this is the case, ocular herpes zoster can affect both eyes as well. As in other locations, the shingles blisters in the eye cause intense PAIN.
The blisters and pain are characteristic of ocular herpes zoster, making it possible for the doctor to make the diagnosis based on their presentation. Treatment typically includes ANTIVIRAL MEDICATIONS (such as acyclovir), ophthalmic CORTICOSTEROID MEDICATIONS to reduce INFLAMMATION, tricyclic ANTI- DEPRESSANT MEDICATIONS to prevent postherpetic NEURALGIA, and ANALGESIC MEDICATIONS to relieve pain. Symptoms may take several weeks to several months to resolve. Numerous complications are possible that can have long-term consequences for vision, including GLAUCOMA and CATARACT. Ocular herpes zoster very seldom recurs, though this is a risk for those who are immunocompromised such as with HIV/AIDS or receiving IMMUNOSUPPRESSIVE THERAPY such as following ORGAN TRANSPLANTATION.
See also BLISTER; CORNEAL TRANSPLANTATION.
ophthalmic examination The basic diagnostic procedures an ophthalmologist uses to assess the health of the EYE and vision, and detect problems with the structures and functions of the eye. The standard ophthalmic examination includes several components. For certain parts of the examination the ophthalmologist may place drops in the eyes that anesthetize the eye and dilate the pupils, to facilitate examining the structures of the back of the eye such as the RETINA and optic disk. Some people experience mild stinging when the drops first enter the eye. There is otherwise no discomfort with an ophthalmic examination. The complete exam takes about 10 minutes.
Physical Examination
The ophthalmologist begins with an examination of the orbital tissues, outer eyelids, inner eyelids, and conjunctiva (membrane lining the inner eye- lids) of first one eye and then the other, checking to see that the eyelids open and close properly and looking for any growths or irritation. The ophthalmologist then checks the movement of the eyes, typically by asking the person to follow the track of an object such as a pen. Using a small light, the ophthalmologist checks the reaction of the pupils. These procedures help the ophthalmologist to assess the basic neurologic aspects of the eye’s functions.
Visual Acuity and Visual Field
The familiar SNELLEN CHART test for VISUAL ACUITY features lines of letters in differing sizes and order of presentation. Covering first one eye and then the other, the person reads the line with the smallest letters that appear clear. The ophthalmologist records the result as a ratio that represents actual visual acuity compared to a standard of 20/20, with a score of 20/20 being what the nor- mal eye sees at a distance of 20 feet. Diminished visual acuity may result from REFRACTIVE ERRORS such as MYOPIA (nearsightedness) or HYPEROPIA (far- sightedness), or signal conditions of the eye such as CATARACT or GLAUCOMA.
The ophthalmologist tests for basic VISUAL FIELD by having the person focus on an object in the distance and signal when he or she can see an object (such as a pen the ophthalmologist holds) that moves into the field of normal vision. This test assesses peripheral vision and helps detect scotomas (small blind spots in the field of vision), which are both symptoms of glaucoma and RETINI- TIS PIGMENTOSA.
Slit Lamp Examination
The SLIT LAMP EXAMINATION, also called a biomicroscopic examination, uses light focused as an elongated slit in combination with magnification. Slit lamp examination allows the ophthalmologist to closely examine the front structures of the eye including the sclera, CORNEA, iris, and LENS. It is a common procedure for diagnosing cataract. The ophthalmologist may also use FLUORESCEIN STAINING to check for CORNEAL INJURY such as ABRASIONS or lacerations.
Ophthalmoscopy
The ophthalmoscope is a hand-held device that resembles a flashlight. It has narrowly focused beam of light and a magnifying lens. The ophthalmologist uses it to examine the inner structures of the back of the eye known collectively as the fundus: the retina, optic disk, and macula. The ophthalmologist usually dilates the pupil for OPHTHALMOSCOPY. This test helps detect numerous problems of the eye including RETINAL DETACHMENT, RETINOPATHY, OPTIC NERVE ATROPHY, and PAPILLITIS.
Conditions such as glaucoma cause characteristic changes to the fundus.
Tonometry
The tonometer is a device that measures INTRAOCU- LAR PRESSURE (the pressure within the eye). The most simple variation involves measuring the force it takes for a puff of air to indent the cornea, a noncontact test. For more accurate results the ophthalmologist numbs the eye with anesthetic drops and touches a TONOMETRY probe against the surface of the eye to measure the pressure. Tonometry is a basic screening test for glaucoma, for which increased intraocular pressure is a key symptom.
See also AMSLER GRID; REFRACTION TEST; SCOTOMA; VISION HEALTH.
ophthalmoscopy Examination of the EYE using an ophthalmoscope, a hand-held, lighted magnifying lens. The ophthalmoscope projects a narrowly focused beam of light that illuminates the structures of the eye. Ophthalmoscopy is the essential introductory examination of the eye and can determine what, if any, further diagnostic procedures are necessary. Ophthalmoscopy allows the doctor to examine the inner surfaces of the eye- lids, general surface of the eye (sclera and CORNEA), pupil response, and iris. It also allows the doctor to visualize the inner structures at the back of the eye, notably the RETINA, optic disk, and macula.
See also OPHTHALMIC EXAMINATION; OTOSCOPY; SLIT LAMP EXAMINATION; TONOMETRY.
optical coherence tomography (OCT) An imaging procedure that noninvasively and painlessly permits the ophthalmologist to visualize the layers of the RETINA. OCT can provide a “virtual biopsy” of retinal tissue, helping diagnose or monitor AGE- RELATED MACULAR DEGENERATION (ARMD), macular
holes, retinal tears, and OPTIC NERVE inflammation or damage such as can result from GLAUCOMA. The ophthalmologist can perform OCT in the office; no preparation or recovery is necessary.
See also ELECTRORETINOGRAPHY.
optic nerve The second cranial NERVE, which conveys nerve impulses from the EYE to the BRAIN. There are two optic nerves, one from each eye. The fibers that become the optic nerve originate in the occipital lobes of the cerebrum, in an area called the visual cortex. Each extends along structures called the optic tracts that pass through the temporal lobes and the center of the brain, con- verging in the optic chiasm. At this point the optic tracts cross, such that the one originating in the left visual cortex goes to the right eye and the one originating in the right visual cortex goes to the left eye. Each optic nerve enters the back of the eye, terminating in the RETINA.
The ophthalmologist can see through the ophthalmoscope the end of the optic nerve, called the optic disk. It appears as a pale circle, about the size of a pencil eraser, against the dark background of the retina. The retina’s network of nerves extends from the optic nerve, gathering nerve impulses from the rods, cones, and other nerve cells in the retina.
For further discussion of the optic nerve within the context of ophthalmologic structure and function please see the overview section “The Eyes.”
See also AGING, VISION AND EYE CHANGES THAT OCCUR WITH; CRANIAL NERVES; ENUCLEATION; OPHTHAL- MOSCOPY.
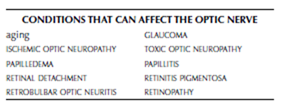
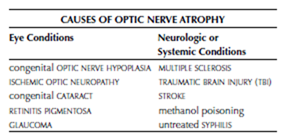
optic nerve atrophy Death of NERVE cells within the OPTIC NERVE, affecting the optic nerve’s ability to convey nerve signals from the EYE to the BRAIN. Optic nerve atrophy can be partial or complete; when complete there is total loss of vision. Conditions of the eye or systemic neurologic disorders can cause optic nerve atrophy. Symptoms include diminished VISUAL ACUITY and VISUAL FIELD.
The diagnostic path begins with OPHTHAL- MOSCOPY, which allows the ophthalmologist to see the visual changes in the optic disk (end point of the optic nerve where it joins the RETINA) that denote its atrophy. Further assessment to deter- mine the cause may include diagnostic imaging procedures such as COMPUTED TOMOGRAPHY (CT) SCAN or MAGNETIC RESONANCE IMAGING (MRI) and a
comprehensive NEUROLOGIC EXAMINATION. Treatment targets the underlying cause, though it can- not recover vision already lost. Treatment that can halt the causative condition can prevent further loss of vision, though when the cause is a degenerative disorder such as MULTIPLE SCLEROSIS vision loss is likely to continue.
People who smoke cigarettes or consume high quantities of ALCOHOL, particularly in combination, have a higher risk for developing idiopathic optic nerve atrophy (in which the cause remains undetermined. NUTRITIONAL SUPPLEMENTS containing vita- min A and the antioxidants LUTEIN and ZEAXANTHIN may improve visual acuity.
See also OPTIC NERVE HYPOPLASIA; RETROBULBAR OPTIC NEURITIS; TOXIC OPTIC NEUROPATHY.
optic nerve hypoplasia A congenital condition in which the OPTIC NERVE fails to develop completely in the unborn child. Optic NERVE hypoplasia is the third leading cause of congenital vision loss in the United States. The defect is random and may affect one EYE or, more commonly, both eyes. Children who have optic nerve hypoplasia may have barely noticeable to complete VISION IMPAIR- MENT depending on the extent to which the optic nerve develops. Diminished peripheral vision and depth perception are common. Typically the pediatrician detects an abnormality of the optic nerve shortly after birth, though mild optic nerve hypoplasia may escape notice until the child begins having vision difficulties. Optic nerve hypoplasia does not progress, so VISUAL ACUITY typically remains stable. CORRECTIVE LENSES may accommodate for vision impairments. Other treatment focuses on teaching the child adaptive methods. There are no known preventive measures.
See also AMBLYOPIA; OPTIC NERVE ATROPHY.
optic neuritis See PAPILLITIS.
orbital cellulitis INFLAMMATION and swelling of the tissues surrounding the EYE, including the eyelids.
Orbital cellulitis requires emergency medical attention. Delayed treatment can result in permanent vision loss.
The most common causes are infections that affect the eyelids such as HORDEOLUM and BLEPHARI- TIS, DACRYOCYSTITIS (infected tear duct), and infections of adjacent structures such as SINUSITIS (sinus infection), PHARYNGITIS (throat infection), tooth ABSCESS, and occasionally OTITIS media (middle ear infection). Insect bites that become infected also can cause orbital cellulitis. Orbital cellulitis may affect one eye or both eyes, depending on the underlying cause. The eyelids typically swell closed and may appear bruised, with considerable PAIN as well as inability to see. Often there is a moderate FEVER (above 102ºF) and EXOPHTHALMOS (bulging of the eye).
The diagnostic path includes assessment of VISUAL ACUITY and VISUAL FIELD, to the extent possible, as well as COMPUTED TOMOGRAPHY (CT) SCAN or MAGNETIC RESONANCE IMAGING (MRI) to visualize the extent of the infection and determine its site of origin. Treatment is immediate intravenous ANTIBI- OTIC MEDICATIONS with hospitalization until fever and swelling subside. Prompt and appropriate treatment improves the likelihood for full recovery and restored vision. Complications can include increased INTRAOCULAR PRESSURE, which is damaging to the RETINA and OPTIC NERVE. Because the optic NERVE presents a direct channel to the BRAIN, INFECTION also may spread to cause MENINGITIS or ENCEPHALITIS.
See also CONJUNCTIVITIS; TRAUMA TO THE EYE.