Hair Restoration Options: Past and Present
In This Chapter
-
Exploring the history of hair transplants
-
Working with smaller grafts and newer techniques
-
Harvesting hair follicles
-
Considering hair cloning possibilities
Serious attempts at replacing lost hair go back more than 50 years, but great strides have been made in achieving a natural
look in just the past few years. Gone are the “plugs” of a decade or two ago; new techniques result in more natural looking hairlines that can make the replacement undetectable.
In this chapter, we look at the evolution of the hair transplant process and explain how the technology, techniques, and skill of today’s surgeons can truly restore your hair. You find out about the options for harvesting hair for transplantation, and we also look to the future and the possibility of hair cloning.
Taking the Long Road to Modern Hair Transplantation
Searching for a cure for hair loss is nothing new, but it’s only in recent years that greater knowledge of genetics and the chemistry of the sex hormones has helped doctors begin to really understand the causes. Androgenic alopecia, also known as male pattern bald- ness, affects more than half the male population to some degree, and it remains the most common cause of balding. Because it also responds well to hair transplantation, hair restoration surgery has gained popularity as a permanent means of addressing genetic hair loss.
Looking at early attempts for a cure
The first documented hair transplant was done in 1822 by J.
Dieffenbach in Wurzburg, Germany. He investigated the concept of auto transplantation (transplanting from one part of the body to another) using hair, feathers, and skin in animals.
Although there were sporadic reports of hair transplantation in European and Japanese literature during the mid to late 19th century, the modern era of hair transplantation really began in 1939 with the Japanese dermatologist, Dr. Okuda, who used small grafts to correct various hair loss conditions of the scalp, eyebrows, and mustache.
Dr. Okuda transplanted round grafts of skin containing multiple hair follicles from permanent hair-bearing areas into smaller, scarred recipient sites. He noticed better cosmetic results with slightly smaller punches than larger ones in the recipient area.
Here’s a brief timeline of key steps toward modern hair loss treatments:
-
In 1943, Dr. Tamura treated 137 patients with non-androgenic alopecia of various causes to restore female pubic hair. He noted that single hair grafts produced results almost indistinguishable from the natural growing hairs. He also noted that larger grafts produced a very unnatural appearance. Due to World War II, the Japanese doctor’s findings remained unknown to the Western world.
-
In 1952, Dr. Orentreich performed the first hair transplant for male pattern baldness. Seven years later, he coined the term “donor dominance,” which is the basic principle of hair transplantation that hair grafts from the back and side of the head (donor sites) continue to grow hair when they’re transplanted to a bald (recipient) site.
-
In 1975, a dermatologist and hair transplant surgeon, Dr. O’Tar Norwood, building upon earlier work, developed a classification of male pattern hair loss that’s still widely used today. (You can find more about the Norwood classification system in Chapter 4.)
Tracing the evolution of hair restoration techniques
Hair transplantation began in the United States in the late 1950s. When doctors examined bald men, they could see that there was hair on their heads but it was just located in the wrong places. So
doctors became very creative in finding ways to redistribute the hair. In this new field, they used tools adapted from other procedures that dermatologists and surgeons commonly performed at the time.
This section explains the three procedures targeted the removal of part of the bald portion of the scalp and rearranging the existing hair.
Punching out plugs
One of the most popular instruments used in early hair transplants was a circular biopsy punch measuring between 3-4 mm. Readily available, it became the standard way to remove donor tissue
from the back of the scalp for the transplant. This hair-bearing tissue was referred to as a plug and soon gained both positive (physiologic) and negative (aesthetic) connotations.
Because these plugs were large, skin had to be removed from the front of the scalp (the recipient area) to make room for them. In fact, the same size punch used to remove tissue from the back of the scalp was also used to remove bald skin from the front. It was replaced with hair-bearing circles of skin from the back and sides of the head where the hair was permanent.
This punch graft technique was the standard procedure for all hair transplants for many years. It was responsible for the extremely noticeable “pluggy doll” look that people commonly associate with the older hair transplant procedures.
Flapping it over
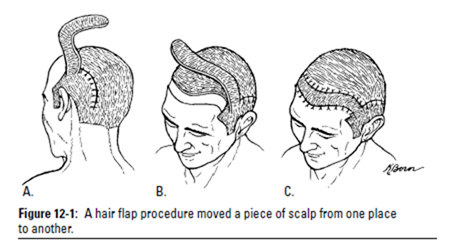
Rather than punching out pieces of scalp and moving them around, an Argentine plastic surgeon, Dr. Jose Juri, had the idea of directly rearranging the scalp by moving one part of it to another.
He would partly incise a banana-size piece of hair-bearing scalp, keeping one part of it connected to its blood supply. Within a few weeks, the healed flap of skin could be lifted up and moved, provided that the blood supply was maintained on one edge.
The flap was rotated so that the hair-bearing skin covered an area of bald scalp that was removed to make room for the flap (see Figure 12-1).
The defect in the scalp at the donor area was repaired by stretching the hairy sides of the scalp almost to the ears and pulling the two sides together to close the defect, and if the defect could not be closed, the wound would be left open to close on its own.
 This procedure had the following advantages:
This procedure had the following advantages:
-
The results were instantaneous. Other than the time between the first surgery to create the flap and the second one to relocate it, there was no waiting around for hair growth.
-
A hairline with thick hair was created when the flap was secured in its new location.
These advantages may make the procedure sound appealing, if perhaps a bit macabre (moving pieces of scalp around your head?). Unsurprisingly, there were many problems with flaps, including the following:
-
Unless the surgeon was very experienced, the blood supply to the flap could fail, leaving the patient with part or all of the flap dying in its new location in the recipient area.
-
The wounds at the recipient site were often a problem, creat- ing a bald area where there was formerly hair. The new bald area often scarred heavily, sometimes with the appearance of an elevated keloid-type scar or just a scar along the edge of the flap.
-
The hair didn’t grow forward, as natural hair in the bald area would have grown. It often grew to the side, or even backward because it maintained its original hair direction in the flap.
-
There was a distinct change from the hairless forehead to a heavy line of thick hair and then, if the patient had any degree of baldness behind the flap the ‘island’ of flap would be easily seen.
-
Unlike a natural hairline, which has a slow transition from the bald forehead to the thicker hair area behind it, the flap had a detectably abrupt hairline and then an abnormal transition to baldness on the back side of the scalp.
-
One flap couldn’t cover the entire reconstructed frontal hair- line, so two flaps were often used and joined in the middle or off to one side. This produced two open wounds in the area it was taken from (one on each side), two directions for frontal hair growth, and a small (or large) cleft between the flaps.
-
Multiple flaps often weren’t equally positioned, so it wasn’t unusual for the hairline to be off balance, with a shape determined by the surgeon’s need to cover the scalp rather than aesthetics. As a result, the new hairline of many of these patients just didn’t look right.
-
The flaps were relatively permanent after they were created.
The patient had to live with the results, like it or not.
Moving to the scalp reduction technique
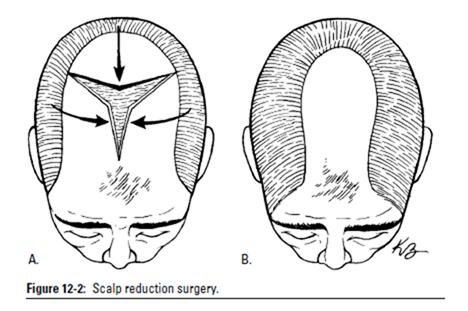
The first of the creative solutions to the problems with the flap technique (see the previous section) came in the late 1970s with the scalp reduction procedure for the treatment of balding in the crown area. The procedure was defined by Dr. Blanchard and
Dr. Bosley commercialized this technique and published the first large series of scalp reductions. With a business focus, Dr. Bosley created his own terminology for the procedure, calling it male pattern reduction.
The essence of this surgery was removal of the bald spot in the top and back of the head. After the bald spot was removed, the surgeon lifted the entire scalp off the head to gain looseness and then attempted to pull the scalp together from the sides to close the defect. Sometimes the defect was too wide to close, so the patient would have only part of his balding spot removed and would return for more surgery some months later. See Figure 12-2.
With a bald area 6 inches wide, it may have taken six or more surgeries to cut out the entire bald area, and the patient was left with an ugly scar where the scalp was put back together. Sometimes more surgeries were required to address stretched scars, and as more and more scalp was removed in successive surgical procedures, the hair on the sides of the head became stretched, reducing the density of the side hair.
 The procedure didn’t even solve the problem of a bald crown, instead placing a scar in a bald of otherwise normal scalp. This led patients to need hair transplants just to cover the scar and make the crown appear normal.
The procedure didn’t even solve the problem of a bald crown, instead placing a scar in a bald of otherwise normal scalp. This led patients to need hair transplants just to cover the scar and make the crown appear normal.
The scalp reduction surgery was a radical, yet a simple procedure, and the number of surgeries performed spread like wildfire. It could be done in under 30 minutes and cost only $1,500 to $3,000. So the scalp reduction flourished among some cosmetic surgeons, who seemed to forget that patients were paying for the removal of their bald spots with pain, suffering, deformities (see Figure 12-3), and seemingly never ending surgeries.
Although thought to be an attractive solution for the bald male at the time, scalp reduction surgery has since fallen out of favor due to high complication rates, high failure rate with bald spot recurrence, poor aesthetic results, and a disgruntled patient population. This procedure brought out the worst of the doctor’s greed for the high surgical fees.
Dr. Mario Marzola tried to improve upon the scalp reduction by dissecting the scalp down to the level of the ears so that more of the lifted scalp could cover a wider defect. With his ability to stretch the sides of the scalp, he was able to remove a wider area of bald skin so the patient would, in theory, require less surgeries. In 1983, he performed the first scalp lift, but to maximize the amount of bald area he removed, he had to cut the nerves on the sides of the head leaving the entire scalp without feeling. Definitely not an acceptable side effect.
Finding ways to produce more natural results
In spite of many missteps, the drive to develop better surgical techniques to move hair around the head led to procedures that were more cosmetically beneficial for the patient.
The usefulness of very small grafts (called micrografts) in hair transplantation was first recognized in the early 1980s. These grafts of a few hairs each were mostly limited to placement in the very front of the hairline because of considerable difficulties in handling and placing them into the bald scalp.
A hair transplant that relied entirely on the use of micrografts was first introduced in 1982 in Brazil by Dr. Carlos Uebel. He reduced the size of the grafts (sometimes called plugs), but he wasn’t able to master the graft survival issues. Although he succeeded in making the results look more normal and natural, the survival of the hairs wasn’t great, and the final result looked very thin.
Over the following two decades, transplant surgeons working on ever smaller grafts figured out ways to handle these fragile grafts without killing them. The secret lay in preventing the grafts from drying and in delicate handling during the harvesting and place- ment process. In refining the technique, doctors came to under- stand that moving more hair in the transplant would eventually lead to fuller and better aesthetic results. The technique defined by Dr. Uebel evolved into what’s now called the megasession, large session transplant surgeries.
In 1994, Dr. William Rassman (one of the illustrious authors of this very book) refined the process and published the first medical articles on the megasession. He also started to show off the procedure’s results at medical meetings by bringing patients as part of his academic presentations.
In 1995, he demonstrated that grafting large sessions of small grafts wasn’t just theoretical, but practical by bringing 23 patients to the International Society of Hair Restorations Surgeons meeting; the patients had experienced considerable balding and had undergone transplants with thousands of very small grafts.
In articles published in 1995 and 1997, Drs. Bernstein and Rassman defined what’s now the gold standard in today’s hair transplant field: They developed a hair transplant procedure that could, in many respects, replicate nature by moving hair follicles in their normal anatomical groups of one, two, three, and four hairs — the follicular unit in one or two surgical sessions.
Finally transplanting hair as it grows in nature made the results identical to nature’s own. This technique they defined is now known as follicular unit transplantation (FUT).
The Newest Transplanting Techniques
In hair transplantation, size does matter! In this case, it’s the size of the grafts that make the difference, and smaller is better. To make up for the small grafts with less hair, large sessions of grafts became necessary. In this section, we look at the refinements that have made hair transplants less detectable than ever before.
Avoiding the “hair transplant” look
A bad hair transplant is easy to spot. The uneven, patchy effect of large, pluggy grafts occurs when a surgeon uses larger grafts
containing many follicular units and the spaces between the grafts are wide. As the grafts heal, they contract and create a contrast between the bald skin and the islands or clumps of hair. Ultimately, the patient is left with a scalp resembling a doll’s head.
Larger graft hair transplants took more skin from the scalp, and it produced subtle deformities in the scalp. Skin abnormalities with larger grafts occur for three reasons:
-
The surface of the transplanted skin may not be aligned with the surface of the surrounding scalp. This problem develops in larger hair grafts when the transplanted skin has enough mass to produce the problem.
-
Scar contraction and/or skin dimpling may occur at the recipient site during the healing process. As the grafts increase in size, these abnormalities occur with increasing visibility.
-
As the skin of the graft heals, the melanocytes (the part of the skin that produces pigment) may not recover from the trans- plant process and give the graft a whitish appearance. This is particularly a problem for anyone with a dark skin color.
Hair in its natural state is composed of hair groupings of follicular units that have one to four hairs close together. In nature, the leading edge of one’s hairline is comprised solely of single-hair follicular units with less density than the hair further back on the head. To appear natural, a hair transplant should simulate that look as closely as possible.
To understand the terminology of hair grafts used by different surgeons, hair grafts can be divided into four general categories:
-
A traditional standard graft, or plug, is 3 to 4 mm in diameter and has 12 to 30 hairs.
-
A minigraft is 1.2 to 2.5 mm in diameter and has 4 to 12 hairs.
-
A micrograft is 1.0 to 1.5 mm or less in diameter and has one to three hairs.
-
A follicular unit is a naturally growing group of one to four hair follicles. Follicular units are smaller in size than minigrafts or micrografts containing the same amount
of hair because the hair exit the skin from roughly the same pore on the scalp.
You should discuss the size of the grafts and the planned distribution of the grafts in detail with your surgeon. Some surgeons use larger grafts for some of their work and then use smaller grafts in an attempt to hide the larger grafts. Others only transplant small grafts.
Some hair transplant surgeons invent unusual terms for grafts to make it appear that they have some special, unique knowledge or technique. These terms are intended to imply special variations in graft sizes or an invisible appearance of the grafts. Don’t be fooled by this terminology.
You should be wary when a doctor claims to have a unique technology or technique that no other doctor knows about or uses, unless it’s documented and published in a peer-reviewed medical journal.
Small versus large hair grafts
To meet the demand for natural-looking hairlines, doctors began decreasing the size of hair grafts in the 1980s, because of the following large graft disadvantages:
-
Large hair grafts are more visible during the transition period after transplantation before the hair grows in. Skin deformities show up almost immediately after the hair transplant.
-
Large hair grafts placed in a frontal hairline look pluggy and unnatural when the hair is combed back or to the side. Patients were forced to comb their hair forward and down to hide their hairlines.
-
When large hair grafts are placed behind the hairline or in the crown, they look like patchy clumps of hair (even in the most gifted surgical hands) and these are very difficult to disguise or camouflage.
-
As healing occurs in three to four mm hair grafts, the grafts contract, pushing the hairs in the graft together and increasing the density of the hair within the graft. The hair density within these larger grafts often exceeds the hair density in the donor area, contributing to the pluggy, stalk-like appearance of traditional grafts.
-
Larger hair graft repairs force the patient to undergo multiple transplant sessions in the quest for natural-looking results, and the patient’s appearance can be strikingly unnatural until the work is completed.
It takes four to six days for the buds of new capillary blood vessels to grow into the hair grafts from the surrounding tissue. Until these new blood vessels grow into the graft, the graft’s cells depend upon the surrounding tissue to bring the needed oxygen and nutrients for their survival.
Hair follicle cells have a very high metabolic rate, and they require more oxygen and nutrients than other cells. If the graft is too large, the cells of the follicles in the center of the graft may die before sufficient oxygen and nutrients can reach the center of the graft. The follicles at the periphery of the graft survive because they’re close to the body’s nourishing oxygen and fluids.
When hair finally grows from larger grafts, those in the center die and this creates a doughnut configuration, with hair at the edges and a bald central area of skin. This is one of the numerous reasons why many doctors have changed to the use of exclusively smaller grafts.
Small hair grafts also have some disadvantages.
-
The amount of time and work needed to place tiny grafts is greater than what’s needed with larger grafts.
-
Smaller hair grafts produce a thinner hair appearance, so many more graft units are needed to produce a natural look.
Minis, micros, and more
Minigrafts and micrografts consist of multiple (partial or complete) follicular units along with the intervening skin. This technique solves the problem of the hairs in the center of the graft dying off, but the contraction of the graft in the healing process still produces a denser graft than normally found throughout the scalp.
These grafts also can cause loss of pigment cells, which can be a particular problem for people with darker colored skin.
Although minigrafts and micrografts are a significant improvement over larger hair grafts, they’re not ideal. The idea behind them
is reasonable: to keep the number of hairs in each graft low and spread more hair in these smaller grafts around. But the following problems are common with minigrafts and micrografts:
-
Surgeons may move more hair in minigrafts and micrografts, but these grafts appear clumpy if they’re not limited to the natural growing groups of hair. Focusing on the naturally growing groups and keeping them intact prevents transplants from looking clumpy.
-
Minigrafts and micrografts aren’t harvested with a high powered microscope, so many follicular units are broken apart and the hairs within them are transected during their preparation, which produces significant hair damage and a reduced hair yield.
-
When minigrafting and micrografting is done with a multibladed knife, the hairs within the knife path break up and the naturally occurring follicular units are unavoidably damaged.
-
Micrografts tend to have more skin in the graft, which makes them lose their skin pigment. Even micrografts containing as few as two or three hairs may contain the skin between two follicular units, which is unnecessary.
-
Micrografts look thin when used exclusively over the entire head and may produce inconsistent graft growth. Follicular damage also contributes to this thin appearance.
Many surgeons promote a variant of minigrafts called a double follicular units (DFU), in which two follicular units are used, each containing one to three hairs. The main disadvantage of the DFU is that there’s intact skin between the follicular units, and particu- larly in the dark-haired, light-skinned, or coarse-haired person, the skin produces a small, white scar as well as cobblestoning (irregularities) on the scalp surface.
This is a subtle change, but one that’s visible on close inspection, particularly in bright sunlight. The loudest complaints about such defects come from patients who can see on themselves the points where the transplanted hair exits the skin.
Hybrid grafting techniques
The use of larger hair grafts for the top and non-central portion of the crown and smaller grafts for the frontal hairline and perimeter of the transplant has a variety of names including blend grafting and variagrafting. Although this hybrid approach is detectable on close inspection, it may not be noticeable in a social setting unless the hair is wet or the patient is in bright sunlight. The results from larger grafts are best in patients with curly, white, or blonde hair.
If you have curly or wavy hair, the hybrid approach or the use of DFUs (refer to the previous section for an explanation of DFUs) may be a reasonable way to reduce the costs of the hair transplant. If you have straight hair, such an approach can be disastrous, particularly if your hair color stands out against distinctly contrasting skin tones (for example, you have dark hair and fair skin). All larger graft procedures generally cost less if the surgeon charges by the graft, and the procedures can be performed without the intense labor required for larger sessions of small grafts.
Another disadvantage of larger grafts may become more evident when further hair loss occurs, particularly when recession allows the grafts to be viewed from a different angle. Using larger grafts or DFUs is more a short-term economic fix than a long-term solution, and we don’t recommend it.
Follicular unit transplantation
Follicular unit transplantation (FUT) was the most significant advance in hair restoration since hair transplants were introduced in the U.S. in 1959.
In follicular unit transplantation, hair is transplanted from the permanent zone (from the back and sides of the scalp) into areas affected by balding, using only the naturally occurring, individual follicular units. Drs. Bernstein and Rassman first described this procedure in the 1995 Journal of Aesthetic and Restoration Surgery. Because of its superior aesthetic results, follicular unit transplantation soon became the gold standard for hair transplantation surgery worldwide.
An essential component of FUT is the use of stereo-microscopic dissection — a technique developed by Dr. Limmer in the late 1980s for dissecting micrografts. Applying this technique to FUT, all the follicular units are removed from the donor tissue under microscopic control to avoid damage.
Complete stereo-microscopic dissection increases the yield of the number of follicular units as well as the total amount of hair (upwards of 25 percent). The hair seems to come out of a single hole and that the hairs are bundled together in their naturally growing groups.
The essence of the follicular unit approach to hair transplantation is that the characteristics of the patient’s hair dictate the size of the implant (rather than the doctor or the surgical team). For example, single follicular units are placed in such a way as to create the natural look of gradually increased density as you go further back behind the hairline.
Still, the surgeon determines distribution, hair direction, and the balance between smaller one-hair grafts and larger two-, three-, and four-hair grafts. By preserving both the natural physiologic and aesthetic elements of your own hair, the best cosmetic results can be achieved.
While the term “follicular unit transplant” may be in vogue with most savvy patients and doctors today, not all doctors and their staff have the knowledge or the technical capacity to perform a large transplant made up exclusively of follicular units.
Very few surgeons and practices have mastered the ability to adequately control quality while performing FUT and follicular unit extraction because the learning curve is very slow and the doctor must commit considerable time and money to this endeavor.
Instead, some medical groups may use different graft sizes and hybrid techniques to speed up the process — at the expense of the final result.
Here are some of the many advantages of FUT over mini- micrografting or DFUs:
-
FUT, when placed in adequate quantities, produces a fuller look because the grafts can be of the same size (or even smaller) than micrografts yet contain more hair and less skin.
-
The growth is more consistent with FUT than when the follicular units are split up, and dividing the units increases the risk of follicular injury.
-
Because follicular unit grafts are less bulky than DFUs, recipient wounds heal more quickly. The sites in the recipient area are smaller, making the results look more natural.
-
FUT allows the surgeon to distribute grafts to mimic the way hair grows naturally in the patient’s own scalp.
-
Because of the greater precision of the harvesting process, FUT enables the surgeon to restore more hair using a smaller amount of donor tissue than with minigrafting, micrografting, or DFUs.
-
The skin between the follicular groups is trimmed away when only follicular units are used, and the vital support structures around the unit are preserved. Cobblestoning (irregularities in the surface of the scalp) and depigmentation (the appearance of whitish blemishes on the transplanted skin) are avoided because excess skin in the grafts is removed, making the grafts significantly less bulky and the holes that they’re placed into much smaller.
-
Because of the very small recipient sites, larger concentrations of follicular units may be safely placed into the bald area, opening the possibility of creating a higher hair density in a single session. More density in these recipient sites reduces the necessity for multiple procedures. The patient benefits significantly with less time devoted to hair restoration surgery without sacrificing the quality of the grafts on close inspection.
With the goal of harvesting follicular units from the back of the scalp without a linear scar, a number of doctors began working on a direct extraction technique. In 2002, Drs. Rassman and Bernstein described their technique, called follicular unit extraction (FUE), which we discuss next. This procedure allows the surgeon to remove individual follicular units directly from the donor scalp with a punch of 1 millimeter or less in size instead of a linear donor incision.
This technique, suitable for a select group of patients, eliminates the need for strip harvesting and is a further refinement in FUT. The technology for performing this technique has, at the time of this writing, made significant strides.
Harvesting Your Hair
There are five common methods of harvesting donor grafts, but only two methods — single strip harvesting and follicular unit extraction (FUE) — are used today.
Single strip harvesting
Single strip harvesting removes the donor tissue as a single strip. The strip of scalp is then divided into smaller sections using a dissecting stereo-microscope; it allows total visual control over the procedure and avoids the unnecessary cutting of hair follicles. (We explain stereo-microscope dissection in the earlier section, “Follicular unit transplantation.”) The stereo-microscope keeps potential damage to follicles to an absolute minimum, and doctors can preserve the intact naturally occurring follicular units.
The great advantage of this method is that the tissue is removed from the scalp with minimal blind cutting because of the use of stereo-microscopic dissection.
Advantages of strip harvesting under microscopic control is that there’s a very high hair yield with an experienced team, and the scar usually is detectable only if you cut your hair to a military buzz cut. Other than the scar and a slightly painful recovery period of a day or two, the strip harvesting procedure is more cost-effective and more efficient from a time perspective. Most importantly, the yield of hair is consistently superior to harvesting without the benefits of a high powered microscope.
The FUE technique can also produce superior hair yields, especially with new technology just being developed. The problem with FUE is that it is very taxing on the surgeon doing the procedure and requires intense concentration for prolonged periods of time to perform the surgery. The surgeon’s fatigue becomes a factor when this technique is extended to more than 1000 grafts.
Robotic hair transplantation, presently on the horizon, will use the FUE harvesting technique as its mainstay for harvesting. Robots will not fatigue as humans do when harvesting follicular units and because of this, robot assisted harvesting promises to produce a technology that will be far superior to hair transplantation done by hand.
Follicular unit extraction
Follicular unit extraction (FUE) allows the surgeon to remove individual follicular units without making a linear donor incision and without removing a strip of donor scalp. This technique has evolved into a minimally invasive technique, just like the evolution of surgeries in the brain, heart, joints, prostate, and intestinal areas where classical incisions have been abandoned for most surgeries.
Individual follicular units are extracted directly from the donor area with a punch of less than 1 mm in size. In contrast to the old punch method in which the punch cut out many follicular units in one swipe in order to remove the grafts, in FUE only a single follicular unit of between one and four hairs is removed directly from the patient’s scalp.
-
In the one-step technique, the doctor uses a sharp punch to surround the targeted graft and then pushes it into the scalp to a depth of approximately 5 mm. The edge is grasped with forceps, and the entire graft is pulled out from the scalp.
-
In the two-step process, the skin is cut to a depth of less than 1 mm and then the doctor uses a dull punch to dissect the graft from the deep structures below the skin. The freed graft is grasped with forceps and pulled from the scalp.
The advantage of the two-step over the one-step technique is that the extraction process minimizes (but doesn’t entirely eliminate) injury to the follicles in some patients.
FUE has the following advantages:
-
There’s no linear scar in the donor area. Of course a scar always results from every skin incision, but since scars are very small and scattered in a larger area, they often aren’t detectable even when the hair is relatively short.
-
There are no sutures or staples to be removed. The small donor wounds are left to close on their own with no sutures or bandages, and they heal within a few days.
-
There’s minimal discomfort in the donor area after the grafts are removed.
-
Exercise and athletic activities can be resumed within a week after the procedure is performed.
Following are some of the disadvantages of FUE:
-
Not everyone is a good candidate for this procedure. Not all doctors agree, but we always test our patients first by taking several biopsies using different FUE instruments and viewing the grafts under a microscope to see whether we can harvest the follicular units without significantly damaging the hair follicles. If we see a significant amount of damaged follicles, we don’t recommend this procedure for a patient.
-
It’s more expensive than strip harvesting. FUE is very tedious, and every graft should be individually extracted by the surgeon as opposed to the strip method, in which skin is removed first and grafts are harvested under a microscope, generally by a skilled team of dissectors.
-
For the same number of grafts, FUE takes more time, sometimes over twice the time, when compared to a strip procedure.
-
FUE produces small puncture scars. That means that if you shave your head, you may see small, whitish dots. There’s no linear scar and the stretched scars of a more traditional strip harvest is virtually eliminated. It is very difficult to detect the FUE scars.
-
A large area of the scalp needs to be shaved or clipped very short when a large session of over 600 grafts is performed. Many patients object to this requirement because of the radical change in their hair styling. In small FUE procedures (under 600 grafts), the areas shaved are generally small, and your doctor will try to shave the areas so that they can be camouflaged by existing hair as much as possible until the hair regrows.
We advise patients undergoing small FUE to keep their hair long enough to cover small shaved strips of scalp. In larger FUE procedures, the shaved areas may be too large to be camouflaged after the surgery. This contrasts dramatically to a strip that can almost always be covered by existing hair immediately after the strip harvesting procedure.
-
FUE can produce damage that ranges from cutting of the hair follicles to destruction of vital elements of the graft in the hands of inexperienced surgeons. The percentage of such damage should be under 10 percent, but that’s
still a significant amount considering that in traditional strip harvesting surgery, the follicular units taken from the strip under the microscope are mostly perfect.
The Hype About Hair Cloning
Modern hair transplants can greatly improve your appearance, but they have limitations. You can only transplant as much hair as is available in donor areas, and the older you get, the balder you get, so you need to cover larger bald areas with decreasing amounts of donor hair.
But what if you could clone your hair — have one hair replicated in the lab so that it would produce many hairs? The donor supply would be limitless. As simple as hair looks to the naked eye, it may seem that cloning hair wouldn’t be all that difficult. There’s a lot more to hair, however, than meets the eye. Hair follicles are complex, containing skin cells, fat, blood vessels, nerves, muscles, and glands.
There’s also a lot more to hair cloning; potential methods include genetic engineering of the cells, so you never lose your hair in the first place, as well as developing techniques to multiply your own hair cells; we discuss them all in the next sections.
“Inducing” new hair growth
In the late 1990s, a British scientist named Dr. Jahoda took dermal sheath cells (cells from the lowest part of the hair follicle) from his own scalp and transplanted them into his wife’s forearm. These cells stimulated new hair growth on his wife’s arm, and the cells, when analyzed, contained both of the couple’s DNA. The fact that his DNA was in her forearm conclusively showed that, at least in this one surgery, he had conquered part of the cloning process.
The results of this experiment have two interesting applications for future hair cloning:
-
The dermal sheath cells act as “inducer” cells, inducing new hair growth without having to transplant the whole hair follicle.
-
The dermal sheath cells seem to be immune privileged organs, which means they can be transplanted from one person to another without being rejected.
Even more importantly from a cloning perspective is that “inducer” dermal sheath cells are fibroblasts, which are among the easiest cells to culture. If these cells can be cultured in the lab, a person’s own donor area could potentially serve as an unlimited source of
hair for the cloning process. That’s what everyone wants to hear, but at the time of writing this book, the cloning process clearly isn’t there yet. Look for more advances in this area, though!
Some issues and problems to overcome in the area of hair cloning include:
-
Dermal sheath cells are difficult to isolate.
-
The ability to culture the cells has to be proven.
-
The cells need to grow in the right direction — through the scalp instead of under the skin or downward.
-
It’s not certain that the induced follicles will continue to grow hair after the initial hair growth is shed (normal hair grows in cycles of two to six years).
-
The cultured cells may revert to an undifferentiated state and stop growing hair over time.
-
It’s unknown whether the inducer cells may also induce tumors or encourage malignant growths.
-
FDA testing and approval will take years.
Using genetic engineering to isolate and correct hair loss genes
Rather than replicating a new organism, genetic engineering alters the DNA of a particular cell so that it can manufacture proteins to correct genetic defects or produce other beneficial changes. Genetic engineering involves three steps:
1. Isolate the problem gene(s).
2. Clone (multiply) the gene(s).
3. Insert the gene inside the cell so that it can correct the problem.
The first gene causing hair loss in humans was discovered by Dr. Christiano at Columbia University. She found that individuals with this gene are born with hair that soon falls out (as infant hair often does) but then never grows back. Unfortunately, this isn’t the gene that causes male pattern baldness (which is probably the result of more than one gene), but labs are working to isolate the genes responsible for that widespread condition.
Multiplying hairs
In hair multiplication, hairs are simply plucked from the scalp or beard and implanted into the bald part of the scalp. The idea is that some germinative cells at the base of the hair follicle are pulled out along with the hair, and when the hair is implanted, these cells should be able to regenerate a new follicle at the removal site and produce a grown hair at the implant site.
In other words, one beard hair removed and implanted in the bald scalp would produce a beard hair in the bald scalp and in the removal site.
In theory, microscopic examination of the plucked hair could help the doctor determine which hairs have the most stem cells attached and thus which are most likely to regrow. The procedure is called hair multiplication because the plucked follicles regrow
a new hair, potentially giving an unlimited supply.
In a modification of this procedure, the bulbs of the hair are separated from the shafts and then cultivated in vitro (outside the body). After the cells multiply, they’re injected into the pores of local, dormant hair follicles in the balding area.
There are three areas where stem cells can be found in the human hair:
-
Above the sebaceous gland near the epidermis in the upper 1mm of the hair follicle
-
At the sebaceous gland 2-3 mm down on the hair follicle
-
Just below the sebaceous gland (the bulge area about 3-4mm down on the hair follicle)
The problem with obtaining stem cells with either technique (hair multiplication and modification) is that:
-
The plucked cells are only transient amplifiers (cells that grow quickly but for only a limited amount of time before they die out).
-
The stem cells around the bulge region of the follicle — the ones most important for hair growth — aren’t harvested in any significant numbers and can’t be readily stimulated to produce a hair.

